Neuroimmune Response Could Be Cause of Rapid Deterioration
Around the world, scientists are racing to find ways to combat the symptoms of COVID-19 as the number of global cases surpasses 9 million. Researchers at The University of Texas at Dallas recently pinpointed a potential strategy for counteracting the acceleration of the illness in the lungs.
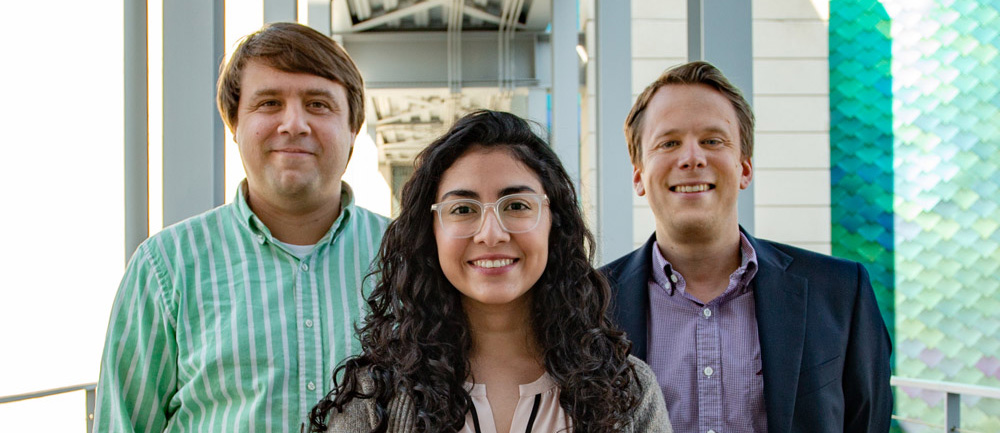
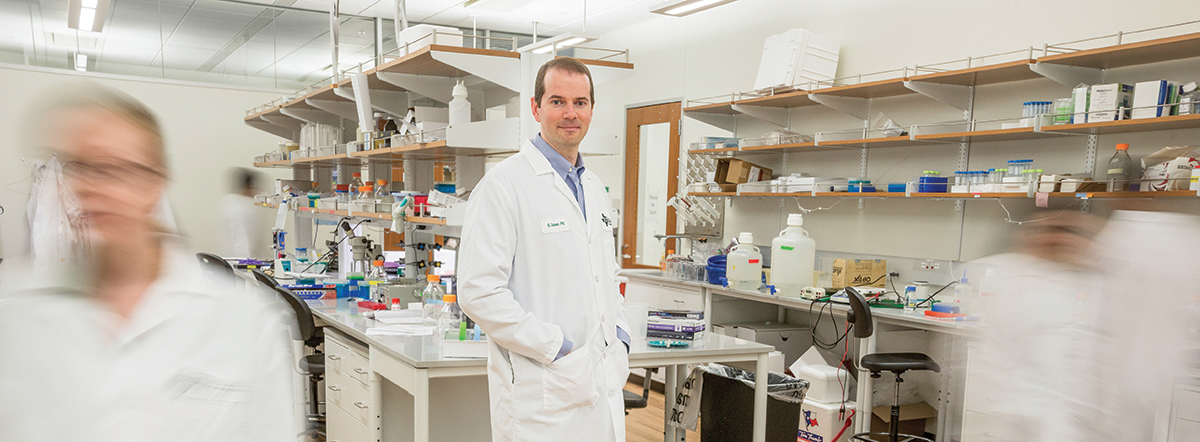
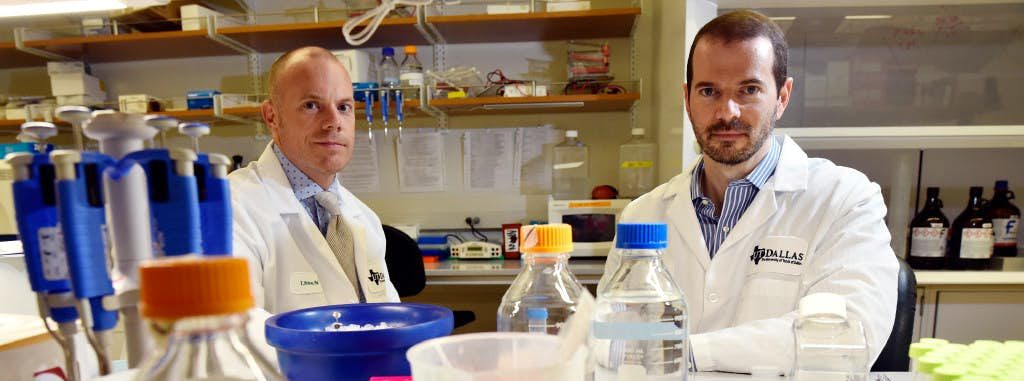
Fourteen scientists from the Center for Advanced Pain Studies (CAPS), a component of UT Dallas’ School of Behavioral and Brain Sciences (BBS), collaborated on a project to determine if the pulmonary issues associated with SARS-CoV-2, the coronavirus that causes COVID-19, could originate with the nervous system.