One of the most exciting, but stressful times of my life is when I realized that I was “ready” to make the transition from post-doc to faculty. Throughout your career, it is imperative to identify mentors that you can have very open and direct conversations with. Interestingly, other people with a good eye will be able to gauge your preparedness better than you can. I remember sitting down with my 2nd postdoc boss and him identifying that I was ready for a faculty position 2-3 years before I felt ready. I knew I would be ready once I hit a certain level of personal training, as well as feeling confident that I could train and mentor individual’s in my future lab space.
Below are a few tips that worked for me. The list is not exhaustive and I’m sure there are plenty of others.
Tip 1. Know your field of interest and the individuals in it.
Where do you have active collaborators? Where can you grow collaborators? Do you have internal support? How do they see themselves versus the rest of the field? And most importantly, do you fit in?
You will need a scientific identity and what you want your lab to be known for. In order for this to be smoother, have the conversation with your postdoc mentor about what you can/want to take with you from their lab to create your own niche. I hope that this is something you have been building for a while…on the side.
Tip 2. Know the environment where you want to go.
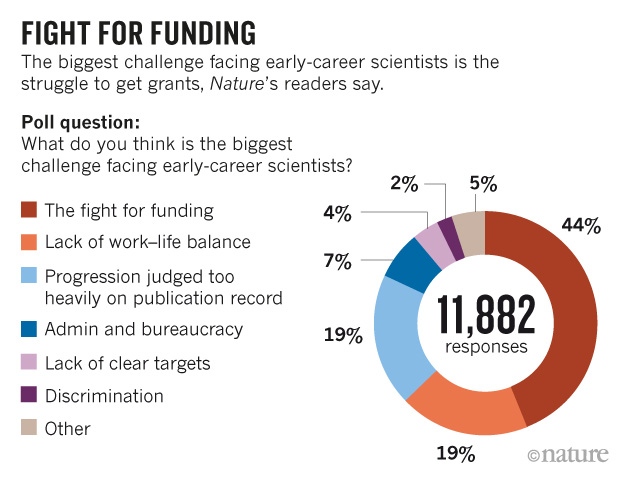
Do you have a desired structure? Do you want to teach undergrads? Do you never want to see undergrads (School of Medicine/Medical Centers)? These environments come with certain pros and cons (mostly salary support for teaching versus grant support). Are you a grant warrior? A teaching aficionado?
Some of the best advice I received while I was on the market was to have a good understanding of the breakdown of salary types (i.e. soft vs. hard; coming from external funds or internally, respectively), but also duration: 9 month vs. 12 months and how you can make that work for your situation. More research protected time, more pay if you have external money etc.
Tip 3. Know your worth and what your lab needs.
Some more great advice I received was that “everything is negotiable…but not everything is worth negotiating.” Knowing an appropriate salary for the department you are entering is very important for you personally, but it is also important to make sure you have an ideal space for your lab (proximity to subjects, ventilation, temperature, humidity, the view).
Knowing what you want and what your lab needs can sometimes mean you sacrifice something in negotiations. But, in general, where you end up should be your biggest fan and be willing to make things work. Do not be afraid to ask, all they can say is ‘no’, you have already been chosen. Your offer will not be rescinded because you ask for a multi-photon scope. But they may laugh at you.
Tip 4. Trust yourself!
You will get an inordinate amount of advice. Don’t get caught up feeling like you have to take everyone’s advice. More than likely you will have to make some decisions all on your own. Trust yourself. You make bad ass decisions, that’s why you are there.
Identify personnel as early as possible. People capital is hard to come by and having well trained individuals in the lab as early as possible will set the lab up. You are great at training and as long as you feel someone is trainable, you can hope to mold trainees.
Tip 5. Find a support group.
Keep a network of newly hired/recently hired PIs at different departments/institutions. Communication with others in your position decreases the isolation feeling…AND the feeling that you’re flubbing it all up! Turns out, you are doing the best you can just like everyone else.
There are many new/young PI workshops that bring people together in the same space. There are Slack pages #NewPIslack, and twitter as well. Don’t be afraid nor think it is a waste of time…it isn’t.
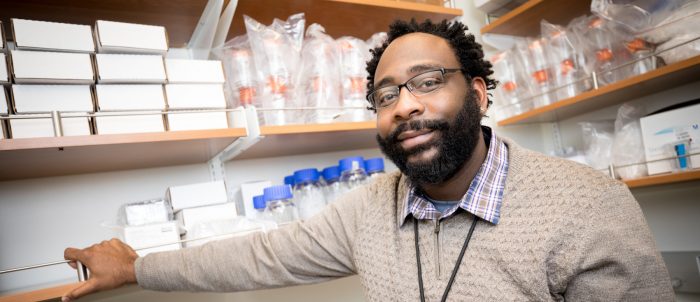
Dr. Michael Burton is an Assistant Professor in the Department of Neuroscience in the School of Behavioral and Brain Sciences. He was recently awarded an NIH-Transition-to-Faculty Award. For more information regarding his research, please visit his lab website.